Is Ketamine an Effective Antidepressant?
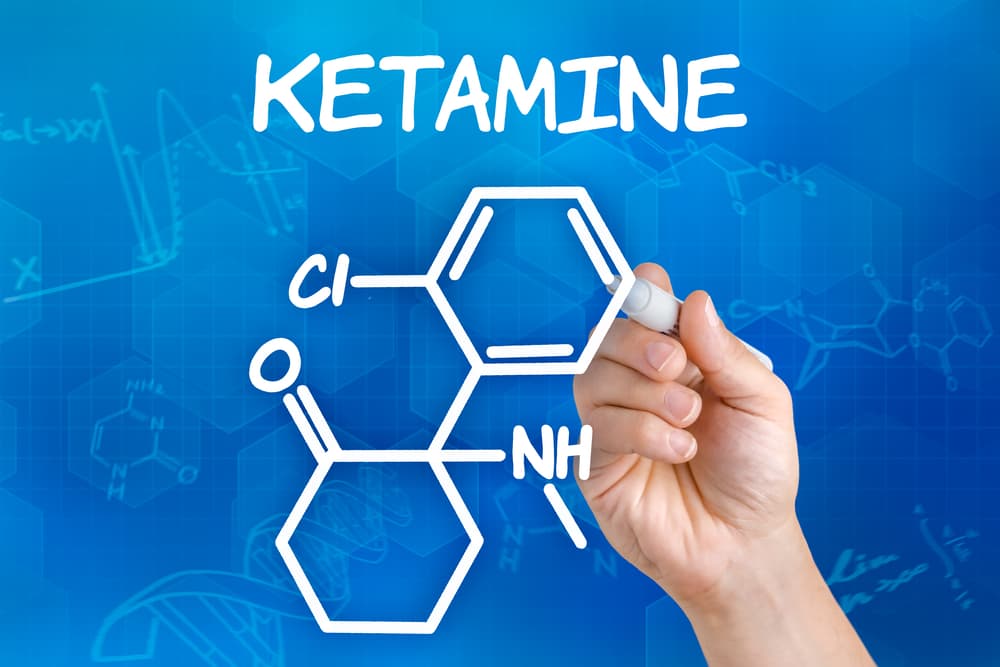
Ketamine, a medication once known primarily as a horse tranquilizer, is gaining attention as an innovative treatment option for depression. This has led to the emergence of services offering ketamine tablets for home delivery. The question arises: what has fueled ketamine’s rise in popularity as an antidepressant, and does it truly work?
Ketamine’s Use in the Medical Field
Despite its reputation, ketamine has a long-standing history in healthcare. It was first created in 1962 and by 1970, had received approval from the FDA for use as an anesthetic. During the Vietnam War, it was utilized to anesthetize soldiers.
Today, ketamine continues to be a valuable asset in hospitals, partly due to its ability to maintain respiratory functions during anesthesia, distinguishing it from other anesthetics.
Research on ketamine as a treatment for depression didn’t begin until 2000. Interestingly, ketamine is one of the only depression medications that was discovered “on purpose” using existing neuroscience research.
The antidepressant effects of most commonly prescribed medications like SSRI’s have been uncovered incidentally. With ketamine, researchers noticed that individuals with depression have an abnormality within the glutamatergic system — the same system that ketamine acts on within the brain.
Since then, a substantial body of evidence has developed showing that ketamine is effective in treating depression.
More than 50% of patients respond to ketamine infusions, which is a much higher success rate than any standard antidepressant used today.
Ketamine is also particularly effective for treatment resistant depression, or cases of depression that don’t respond to other medications and therapies.
Another important indication of ketamine research is that it is extremely well tolerated. The side effects of ketamine treatment include mild nausea, drowsiness, or dissociation that subsides shortly after treatment.
Compared to the strange and widely ranging side effects that can come with most traditional antidepressants, this may be a surprisingly short list.
There aren’t any dangerous or long-term health effects associated with ketamine therapy.
What Makes Ketamine Different from Traditional Antidepressants?
A key characteristic of ketamine that sets it apart from other antidepressants is the duration of its effects.
Studies show that ketamine can begin to reduce depression symptoms as soon as 24 hours after a single infusion.
This is a much faster response than medications like SSRI’s, which can take multiple weeks to have an effect.
Once a ketamine treatment course is complete, the effects can last for many weeks or even months. This is due to ketamine’s unique mechanism of action that causes its antidepressant effects.
Rather than temporarily altering neurotransmitter levels like serotonin or dopamine, ketamine acts on NMDA receptors, which trigger the production of glutamate.
Through a series of complex events, this actually prompts the brain to develop new neural connections — a process known as synaptogenesis.
Ketamine is the only treatment for depression that affects the brain in this way, leading to lasting symptom improvement and long-term change in a person’s life.
Ketamine’s effect on neural pathways makes it ideal as a way to augment traditional psychotherapy.
Coupling talk therapy with ketamine infusions is known as ketamine assisted therapy, and can be a transformative experience for people struggling with depression.
Its dissociative effects often help people remove themselves from emotion, talk about difficult or sensitive topics, and make important realizations during therapy.
Pairing ketamine with therapy can enhance the benefits of both treatments.
Researchers are now looking into using ketamine to treat a variety of other mental disorders, such as PTSD, OCD, ADHD, and anxiety. Initial studies are showing promising results for ketamine as a treatment for these conditions.
For example, this study conducted in 2014 showed that repeated ketamine infusions significantly reduced core PTSD symptoms in individuals with chronic PTSD compared to a placebo.
Improvements were recorded as early as 24 hours after one infusion and remained for 27 days on average.
Although more research is needed to consider ketamine a medically trusted treatment for these conditions, we’re seeing similar findings across the board.
Above all, ketamine treatment is safe, so many individuals are choosing to receive ketamine for these conditions, and are experiencing relief.
Ketamine is Under-regulated
Although ketamine is scientifically backed as an effective depression treatment, regulation around the medication is limited.
In 2019, the FDA approved of one form of ketamine therapy — Spravato, the esketamine nasal spray. Administration of Spravato is standardized in every clinic, but traditional ketamine infusions are still a popular method of administering ketamine, and this method isn’t standardized.
Consumers need to have extreme caution when pursuing ketamine infusion therapy. There are hundreds of clinics that offer the service and treatment can vary widely by dosage and procedures.
In order to ensure that a ketamine treatment will be safe and effective, it’s important to know how to find a reputable ketamine clinic.
A clinic that only offers ketamine or mental health services is the first indicator that they’re trustworthy.
If a clinic offers a wide variety of services such as botox and vitamin infusions, think twice before going there for ketamine treatment.
Similarly, a trusted ketamine clinic will employ a thorough screening process to determine if you’re a good fit for ketamine treatment. If a clinic has a weak screening process (or none at all), to put it simply, run for the hills.
Another red flag to look for is the claims that a clinic makes about ketamine treatment. Yes, ketamine is a groundbreaking discovery in the mental health field, but it isn’t a magical cure.
If a clinic promises to heal you with ketamine treatment, stay away. A clinic should be honest about the pros and cons of ketamine therapy, ketamine’s effectiveness, side effects, and shortcomings.
Always choose a location that has medical professionals and therapists on their team and is ready to work with you to develop a treatment plan that is tailored to your needs.
Ketamine isn’t a one-size-fits-all solution — it should be combined with other modalities to treat your specific symptoms in the best way possible.
References
- Ketamine’s Historical Use and FDA Approval
– [FDA History]
– Patel, R., & Dickenson, A. H. (2016). Mechanisms of the gabapentinoids and α2δ-1 calcium channel subunit in neuropathic pain. *Pharmacology Research & Perspectives*, 4(2), e00205. - Research on Ketamine and Depression
– [NIMH: Ketamine for Severe Depression]
– Berman, R. M., Cappiello, A., Anand, A., Oren, D. A., Heninger, G. R., Charney, D. S., & Krystal, J. H. (2000). Antidepressant effects of ketamine in depressed patients. *Biological Psychiatry*, 47(4), 351-354. - Ketamine and Neural Connections
– [Harvard Review: Ketamine for Major Depression]
– Li, N., Lee, B., Liu, R. J., Banasr, M., Dwyer, J. M., Iwata, M., … & Manji, H. (2010). mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. *Science*, 329(5994), 959-964. - Ketamine Assisted Therapy
– [Psychedelic Science: Ketamine-Assisted Therapy]
– Mithoefer, M. C., Grob, C. S., & Brewerton, T. D. (2016). Novel psychopharmacological therapies for psychiatric disorders: psilocybin and MDMA. *The Lancet Psychiatry*, 3(5), 481-488. - Ketamine for PTSD, OCD, ADHD, and Anxiety
– [Research on Ketamine for PTSD]
– Feder, A., Parides, M. K., Murrough, J. W., Perez, A. M., Morgan, J. E., Saxena, S., … & Charney, D. S. (2014). Efficacy of intravenous ketamine for treatment of chronic posttraumatic stress disorder: a randomized clinical trial. *JAMA Psychiatry*, 71(6), 681-688. - Regulation and FDA Approval of Ketamine
– [FDA Approval of Spravato]
– Popova, V., Daly, E. J., Trivedi, M., Cooper, K., Lane, R., Lim, P., … & Manji, H. (2019). Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. *The American Journal of Psychiatry*, 176(6), 428-438.